7. Arrival at Entrance 6
The main front door should be segregated with the barrier to ensure one route in and one out, the café area must be cordoned off. There will need to be a supply of alcohol gel for patient use on the incoming side and a clinical waste bin and a supply of alcohol gel on the outgoing side.
The patient will be met at the door by a member of our team who will be wearing a mask, gloves, apron and visor. They will determine that the patient is attending for an appointment – either with us, cardiac MRI/CT or cardiology outpatient clinic – no one should be using the route as a thoroughfare and should, if necessary, be directed to another relevant entrance.
The patient's temperature should be recorded:
If it is greater than 37.8°C:
They should be advised to return home and consult NHS 111 if concerned - they must not enter the department.
If it is less than 37.8°C:
The patient should be asked “Have you or anyone you live with had a persistent cough, temperature or tested positive for COVID-19 within the last 14 days?”
If the patient answers Yes, they should be advised to return home, self-isolate as per guidelines and consult NHS 111 if concerned - they must not enter the department.
If the patient answers No, Ask them to alcohol gel their hands and take a seat in the cafe waiting area.
The seats in the waiting area will be set out 2 metres apart to maintain social distancing and should be cleaned down with Clinell wipes when the patient is called in for their appointment.
8. The stress echo appointment
The SE team should all wear the following PPE - apron, gloves, fluid resistant surgical mask and visor, which should be donned and doffed appropriately. This PPE should be worn to collect the patient from the cafe waiting area. Follow the one way system in the department to bring the patient to the clinic room.
Before starting any stress echo lists, each member of the team should ensure that there is full PPE (long sleeve gown, FFP3 (Fit tested) mask, gloves and visor) readily available in the clinic room for each team member to don in the event of a cardiac arrest (in addition to the PPE already on the resus trolleys). If any team member swaps into a list at any point it is their responsibility to make sure there is an appropriate FFP3 mask available for them.
On the way through the sub-wait, invite the patient to gel their hands.
Once in the room, the nurse will gain consent from the patient for the test to be performed, following discussion and explanation of the procedure, including reference to the amended SOP for cardiac arrest during Covid-19.
Record the patient’s height and weight. The patient should be given a gown and mask to wear.
Connect ECG and blood pressure monitoring equipment (if possible put the BP cuff over the gown). This should be monitored continuously throughout the test. Record a resting BP reading and document this. If resting BP is greater than 220/120mmHg then wait a few minutes and recheck. If the BP remains at > 220/120mmHg the test must be aborted.
Perform peripheral venous cannulation and ensure patency.
Ascertain the target heart rate that is to be achieved, if required (HR table is displayed on the wall in all stress rooms).
Obtain baseline echo images and make an assessment of resting LV function, any valvular disease. Exclude severe aortic stenosis.
Determine the need for contrast whilst obtaining baseline data. Contrast should be administered at each image acquisition stage if 2 or more segments of the left ventricle can not be clearly visualised on the non contrast images.
ICP checklist discussion immediately pre-procedure to clarify protocol;
- Dobutamine Stress Echo Protocol - Ischemia Study
Select the stress protocol on the machine, turn on the contrast setting if required. Acquire baseline protocol images and begin dobutamine infusion starting at 5mcg/kg/min followed by 10, 20, 30mcg/kg/min (40mcg/kg/min in rare circumstances) at three minute intervals until target heart rate is achieved (see diagram below);
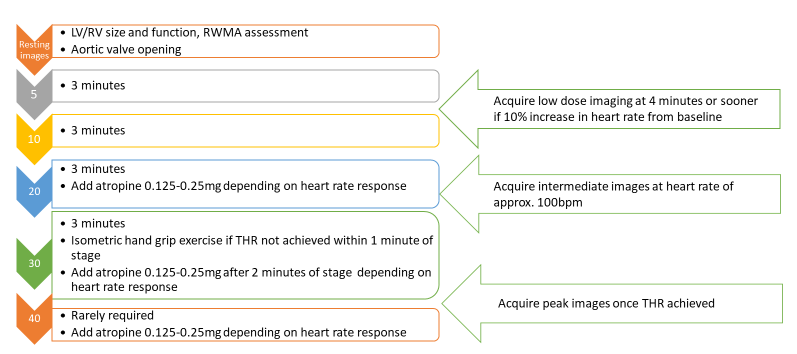
Doses of Dobutamine expressed in mcg/kg/min. Maximum dose of 1.2mg atropine should be administered. If nearing target heart rate and using atropine, start with small (0.15mg) aliquots due to potential to ‘overshoot’ target heart rate (makes image interpretation more challenging). If the patient starts to exhibit vagal response, introduce atropine early and ask the patient to perform leg raises.
End points/termination of the test are achievement of target heart rate (85% of the age predicted maximum heart rate), new or worsening wall motion abnormalities of moderate degree, significant arrhythmias, hypotension, severe hypertension and intolerable symptoms.
- Dobutamine Stress Echo Protocol - Viability Study
Select the stress protocol on the machine, turn on the contrast setting if required. Acquire baseline protocol images and begin dobutamine infusion starting at 5mcg/kg/min followed by 10mcg/kg/min at five minute intervals. Stop after low dose imaging (10mcg/kg/min).
If however ischemia assessment is required and significant LV contractile reserve is demonstrated proceed to high dose ischemia protocol and target heart rate (see diagram below). Please note a higher level of caution should be used during COVID-19 when proceeding to high dose Dobutamine protocols after viability studies, if in doubt do NOT proceed.
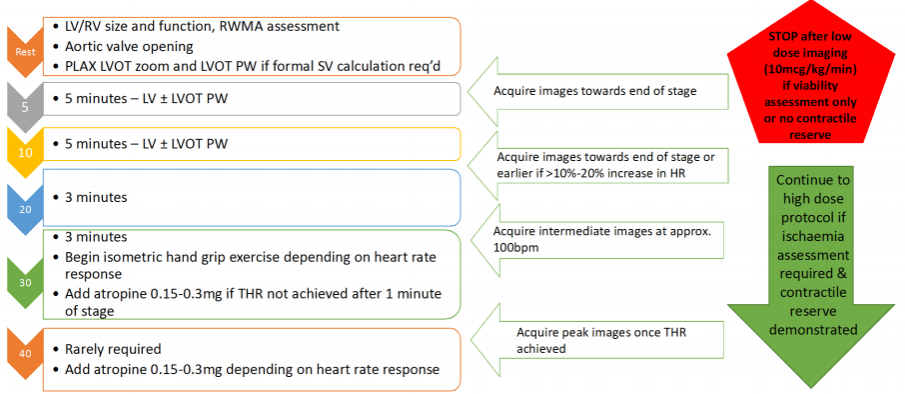
Doses of Dobutamine expressed in mcg/kg/min. Maximum dose of 1.2mg atropine should be administered. If nearing target heart rate and using atropine, start with small (0.15mg) aliquots due to potential to ‘overshoot’ target heart rate (makes image interpretation more challenging). If the patient starts to exhibit vagal response, introduce atropine early and ask the patient to perform leg raises.
In the event of a contrast reaction the test must be immediately terminated and the allergy protocol/anaphylaxsis protocol must be followed (these are on the wall in the stress room).
If a cardiac arrest is confirmed at any point during the test, pull the emergency buzzer and follow the SOP for cardiac Arrest in Patients in the Cardiac Diagnostic Centre During the Covid-19 Pandemic and the Resuscitation Council ALS Algorithm for Covid-19 Patients.
Please note, once cardiac arrest is confirmed the physiologist should remain with the patient and apply the defibrillator pads and deliver up to three stacked shocks, if required, as per the cardiac arrest guidelines, while the rest of the team don full PPE (gloves, long sleeved gown, FFP3 (FIT tested) mask & visor).
Once the team has donned full PPE, the physiologist can then step out of the room and don full PPE. Do not commence CPR (chest compressions and ventilations) unless ALL staff members in the room are all wearing gloves, long-sleeved gown, FFP3 mask and visor.
Following completion of either the ischemia or viability DSE protocol, allow the patient a period of recovery until baseline state is achieved and 30 minutes has elapsed since contrast was administered (to ensure no late contrast reactions). Contact the imaging consultant via phone to review images remotely and complete the report where possible in the clinic room.
If required, to avoid any potential delays in transport causing patients to wait around outside the building for their lift, allow the patient to ring their driver ~15 minutes before leaving the clinic room. If the patient has driven to the appointment by themselves however and has had Atropine they are not permitted to drive for 2 hours and so must wait in their car/outside until they are safe to drive - they are not permitted to wander around the hospital.
When the patient is ready, invite them to gel their hands and direct them out of the echo department via the door beside Echo Room 5, and point them in the direction of the exit (there are arrows on the wall).
Explain to them that before exiting the building they should re-apply alcohol hand gel.
You must then clean down the remainder of the room – examination couch, patient chair, scanning chair, etc.
Remove your PPE as per protocol, clean the visor, wash your hands and leave in the room.
Associated Trust documents
- Standard Operating Procedure for Cardiac Arrest in Patients in the Cardiac Diagnostic Centre During the Covid-19 Pandemic
-
Resuscitation Council ALS Algorithm for Covid-19 Patients.
-
MFT Infection & Prevention Policy
-
British Society of Echocardiography guidelines