
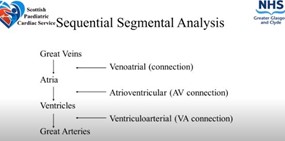
Taking the segmental approach to imaging congenital heart disease (CHD) enables everyone to talk the same language and ensures optimum management.
 |
| Figure 1: Stages of evaluation and imaging modalities in cardio-oncology |
Dr Lindsey Hunter, Consultant Paediatric and Fetal Cardiologist, at the Royal Hospital for Children in Glasgow, said: “You have to be methodical in your report, stepping through the heart piece by piece, as missing out an important anatomical feature can change the diagnosis and management significantly.” She said that any additional abnormalities should also be reported.
By following the standard sequence of segmental analysis (see fig 1), sonographers can ensure their reports are clear and understandable.
Dr Hunter gave the conference a step-by-step guide to performing and reporting a segmental analysis.
- Cardiac location and situs:
- Specify position and orientation of the heart within the thorax: Orientation refers to the right to left, or base to apex axis, position of the heart. Apex to the left should be described as levocardia. If the heart is in the mid-line, or vertical, it is defined as mesocardia, and apex to the right is dextroposition.
- Specify the position of the abdominal viscera (abdominal situs): The heart and the abdomen are asymmetrical, and symmetry could be a sign of abnormality. Many of these images are taken using subcostal imaging, but when children and babies spend a long time in this position, it can result in decompensation or desaturation. During imaging, the probe should be in the 3 o’clock position, the liver should be on the right, and the stomach on the left.
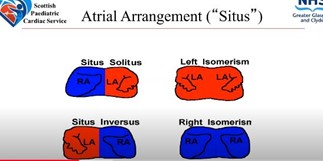
- Specify the position of the atria (atrial situs): This is a description of where the atria are positioned (see fig 2).
 |
| Figure 1: Stages of evaluation and imaging modalities in cardio-oncology |
- Venous segment
The venous segment includes the veno-atrial connections, and the great veins and pulmonary veins to the atrial mass. Sonographers should image:
- Systemic venous connection: The inferior vena cava (IVC) and the superior vena cava (SVC) should connect to the right atrium. This can be imaged using subcoastal, substernal notch, or high parasternal view. The anatomy of the coronary sinus and hepatic veins is also important.
- Pulmonary venous connections: Understanding pulmonary venous drainage can be challenging, but colour flow and 2D echo are both very important when delineating the anatomy.
- Atrial segment
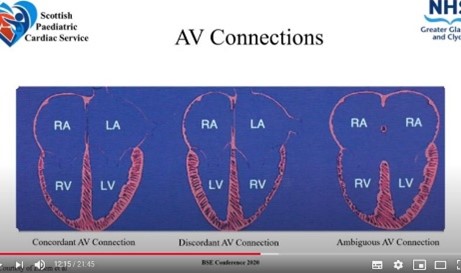
Analysis of the atrial segment centres on examining the atrioventricular (AV) connections. Dr Hunter recommended an apical four-chamber or subcoastal view to determine if the AV connections are:
- biventricular or univentricular: This is usually plain to see by the size of the ventricles, but sometimes the ventricles are borderline in size.
- concordant, discordant, or ambiguous: This is determined by looking at the offsetting of the AV valves. The tricuspid value should be more apically placed than the mitral valve and there should be a moderator band in the right ventricle (RV) (see fig 3).
- When describing the AV connections, two inlets opening into one ventricle is classed as a double inlet, and an absent right or left AV connection a single inlet. When one common valve opens into the ventricle, this should be called a common inlet on reports. It’s also important to describe if the ventricle the valve is opening into is a dominant right or dominant left, said Dr Hunter.
 |
| Figure 1: Stages of evaluation and imaging modalities in cardio-oncology |
- Ventricular segment
Ventricular arterial (VA) connections are the focus during ventricular segment imaging. It aims to determine whether circulation is biventricular or univentricular, and looks at right ventricle (RV) versus left ventricle (LV) morphology.
- Sonographers should record whether the connections are concordant, running from LV to aorta, and RV to the pulmonary arteries (PA), or discordant, with LV connected to PA and RV to aorta.
- The great arteries should cross each other, and not arise in parallel.
- Great arteries
This final stage of the segmented approach to imaging in CHD is the examination of the great arteries. Sonographers should:
- Use the short axis view to check that the coronary arteries arise from the trileaflet aortic valve (en face), and the pulmonary valve/PA from the RV.
- Use 2D and colour-flow Doppler to assess the pulmonary valve size, any stenosis, or abnormal orientation.
- Visualise the confluent branch PAs in the short axis by rotating the probe to 3 o’clock.
- Move to the suprasternal notch to look at the aortic arch. Dimensions, head and neck branching patterns, and whether it sits to the right or left of the trachea are important to note.
Summing up, Dr Hunter said it was important to describe the anatomy, function and physiology of each segment, as well as any abnormalities, in an echo report.
“The description should be methodical, but the scan may be taken in a variety of orders, depending on your patients age and cooperation. But as long as you can communicate your findings to your team and they are able to understand the anatomy that you are describing – that is the most important outcome,” she said.
BSEcho 2020 presentations are available on our website for members of the Society.
View the presentations