It is well recognised that the closer to the patient it is possible to perform a diagnostic test then the more likely it is that the test will be successfully undertaken (e.g. mobile mammography units for breast cancer screening).
However, this desire to minimise the friction present between the patient and access to the test has to be balanced against an ability to deliver a high-quality and safe service, one that is able to produce a report of maximal clinical utility. This issue is particularly important in the provision of community echocardiography given the high level of initial training and ongoing effort to maintain expertise that are needed to both obtain images and report these scans.
It can only be a good thing for patients that they are given quicker and more efficient access to high quality echocardiography after this test has been requested. However, in order to deliver this service in the community (i.e. at a site remote from the immediate support and backup of an in-patient hospital facility) certain aspects of the provision of any good echocardiography service become even more critical. At their core, the key dependencies required stem around ensuring excellent, free-flowing communication between all healthcare staff and safeguarding the community echocardiographers so that they do not work in isolation but are instead an integral component of the wider local cardiology infrastructure. These features of a high-performing service have also been endorsed by the recent NHS England Cardiology GIRFT Programme National Specialty Report1, through its recommendation for the creation of regional Cardiology ‘Managed Clinical Networks’.
The key safety net items to consider in a community echocardiography service are:
- Clinical standards
The BSE has produced extensive guidance to assist with the creation and ongoing running of an effective echo department. This includes advice around audit and quality assurance2, triage of referrals3 and important estates and personnel dependencies described in the departmental accreditation process4. It would be expected that any community echocardiography service hoping to adhere to best practice would follow this well established guidance.
- Adequate supporting Information Technology (IT) infrastructure
It is important that real-time echo-image transfer is available from the community site to the networked local cardiology service. This ensures that even when community echocardiographers are working in physical isolation, they always have access to a second ‘pair of eyes’ to allow for co-reporting of difficult cases and avoids the unnecessary duplication of scans as patients transfer between healthcare settings. It is recommended that the same IT solution is in operation across the networked local cardiology service, and it is possible that funding will be made available in the future to facilitate this element of the digitisation of diagnostic care5. However, if this is not possible then an appropriate mechanism to allow for real-time encrypted transfer of images between sites should be in place.
- Escalation pathways for predictable medical problems
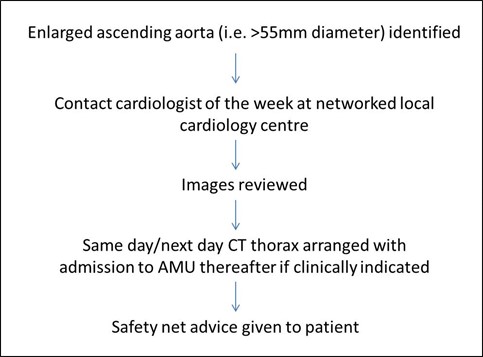
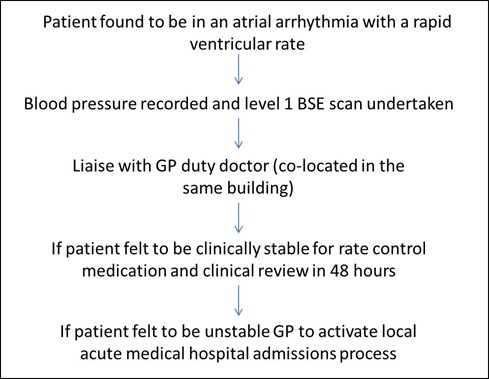
Despite triage of referrals, it is recognised that patients in whom an echocardiogram is requested are a potentially high-risk group and so may arrive for their scan unwell or have an issue identified during the scan which requires prompt medical attention. Accordingly, no community echocardiography service should operate without a set of clear standard operating procedures (SOP) in place that outline the plan to be followed should certain predictable medical issues be picked-up during an appointment. The range of SOPs recommended is not limited to the examples outlined below, but at a minimum must clearly describe how the following foreseeable medical problems are addressed:
- Patients found to be in an atrial arrhythmia with a rapid ventricular rate (i.e. >120bpm)
- Possible type A aortic dissection (i.e. non-coronary cusp associated) or aneurysm of the ascending aorta identified during the scan
- Unknown symptomatic severe left ventricular systolic dysfunction
- Unknown symptomatic severe valvular dysfunction
- Unknown second or third degree heart block
- Unknown cardiac tumour, mass or thrombus
- Unknown significant pericardial effusion
- Possibility of acute endocarditis
Where same day medical input is required, it is insufficient for the community echocardiographer to simply create a report asking for the referring doctor to arrange this. Neither is a blanket statement such as ‘call 999’ adequate as this will almost certainly result in unnecessary and potentially avoidable patient distress as they navigate between healthcare settings. Creation of these SOPs will require granular level input from the wider local cardiology network and other key stakeholders if necessary (e.g. local ambulance services). Lastly, it is important to emphasize that other than training in immediate life support, echocardiographers are generally not qualified to deal with medically unwell patients. Accordingly, a lack of planning around how to address a set of predictable (if uncommon) medical scenarios could result in significant and unnecessary stress being placed upon a community-based echocardiographer.
Example SOP escalation pathways (details dependant on agreement between all parties and local resources):
- Support for sonographers
It is essential that echocardiographers working in a community setting do not only work in this environment but instead rotate through the site with time spent in other parts of the local cardiac service network. This movement of personnel ensures that best practice is spread throughout all team members. In addition, it is expected that people working in a community echocardiography setting are allowed sufficient time in their job-plan to attend local departmental echocardiography governance meetings. Support should also be available to assist echocardiographers with travel between sites.
In setting up a new community echocardiography service, if it is anticipated that a greater number of scans are to be performed overall (rather than simply shifting the location where they are performed) then an increase in workforce must be in place before the service can begin. In addition, prior experience demonstrates that when an existing echocardiography department is required to provide a new community echocardiography service then the overall efficiency of that department will decrease. This is because the institution of split-site working removes the ability to nimbly rotate staff at short notice when unforeseen problems arise.
- Accommodating trainee sonographers
All centres that undertake community echocardiography should accommodate trainee echocardiographers. It is expected that these trainees will not be able to cover the entire breadth of the BSE level 2 syllabus in the community setting and so will rotate though this environment alongside time in other parts of the local cardiac service network.
In summary, the responsibility for addressing the critical components outlined above is collective and lies with all stakeholders within the local cardiac network. In point of fact, it is this collaboration that is the most essential component to ensure that a community echocardiography service can thrive.
BSE Council December 2021
References
- Cardiology - Getting It Right First Time - GIRFT
- The Echocardiography Quality Framework: a comprehensive, patient-centered approach to quality assurance and continuous service improvement in: Echo Research and Practice Volume 5 Issue 4 (2018)
- Clinical indications and triage of echocardiography posters
- Departmental accreditation
- £250 million in NHS technology to modernise diagnostics - GOV.UK